Heading 2
No Pressure
Published on 16 November 2020
NHS Western Isles is delighted to support ‘Worldwide STOP Pressure Day’, this year being held this coming Thursday (19th November 2020).
With approximately 412,000 people likely to develop a new pressure ulcer annually in the UK, which presents a significant burden on healthcare provision in the NHS, the event is organised by the European Pressure Ulcer Advisory Panel and aimed at raising awareness of pressure area prevention.
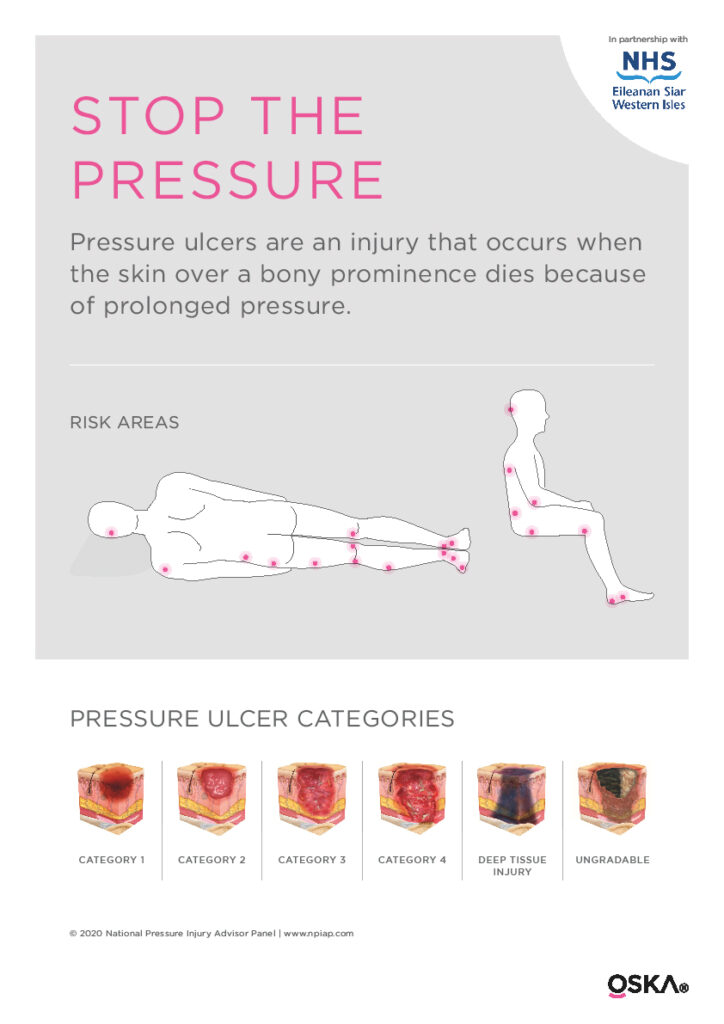
Rosemary MacRitchie, NHS Western Isles Clinical Nurse Specialist Tissue Viability & Continence Advisor, said “It is vital that islanders are aware of pressure ulcers and the harm they can cause. Sometimes known as “bedsores" or “pressure sores", pressure ulcers can range in severity from patches of discoloured skin to open wounds that expose the underlying bone or muscle.
“Although those aged over 70 years are particularly vulnerable, pressure ulcers can affect anyone at any age and I would urge anyone who has any symptoms or concerns to make an appointment with their GP at their earliest convenience.”
What is a pressure ulcer?
A pressure ulcer is damage that occurs on the skin and underlying tissue and is caused by any of the following:
- pressure – the weight of the body pressing down on the skin
- shear – the layers of the skin are forced to slide over one another or over deeper tissues for example when you slide down or are pulled up, a bed chair or when you are transferring to and from your wheelchair.
- friction – rubbing the skin
The most common places for pressure ulcers to develop are over bony prominences (bones close to the skin). This includes the sacrum, heels, elbows, hips and spine, but can develop anywhere.
Anyone can get a pressure ulcer, but some things which can make them more likely to form include:
- being over 70 – older people are more likely to have mobility problems and have skin that is more easily damaged through dehydration and other factors
- being confined to bed with illness, or after surgery
- inability to move some or all of the body (paralysis)
- obesity
- incontinence
- a poor diet
- medical conditions that affect the body’s blood supply, or make the skin more fragile or cause movement problems e.g. peripheral arterial disease, diabetes (particularly with peripheral neuropathy), heart failure, Multiple Sclerosis, kidney failure and Parkinson’s disease.
Pressure ulcers can develop gradually or can appear in less than an hour. The early symptoms of a pressure ulcer may include:
- part of the skin becoming discoloured – people with pale skin tend to get red patches, while people with dark skin tend to get purple or blue patches
- discoloured patches not turning white when pressed
- a patch of skin that feels warm, spongy or hard
- pain or itchiness in the affected area.
Tips to prevent pressure ulcers
Keep Moving – one of the best ways of preventing a pressure ulcer is to reduce or relieve pressure on areas that are vulnerable to damage. You can do this by moving around and changing position as much as possible. If possible, you should change your position at least every two hours; alternating between your back and sides.
However, if you already have a pressure ulcer, lying or sitting on the ulcer should be avoided as it will make the ulcer worse. People with limited mobility may need assistance to change their position from a healthcare professional, carer or family member. You may also require a special mattress, special offloading devices for feet, or a seat cushion, all of which your healthcare professional can advise you on what would be suitable to your needs.
Skin Assessment – your skin should be assessed regularly to check for signs of pressure ulcer development. How often your skin is checked depends on your level of risk and your general health. You or your carer should inspect your skin for signs of pressure damage – remember that you may need help to look at more awkward areas, such as your bottom or heels. If you are Diabetic (or someone you are caring for is) remember the Touch the Toes test, as those with neuropathy (numbness) are at an increased risk.
A good diet – eating well and drinking enough water is very important, and particularly important for people at risk of developing a pressure ulcer, or those who have a pressure ulcer. Please note that if you already have a pressure ulcer, your body will require extra calories to heal.
Eating foods high in calories and protein, such as cheese, fish, meat and eggs, can help. If you do have a pressure ulcer, you (or a healthcare professional), can self-refer you to a Dietician at the Department of Nutrition and Dietetics for specialist advice.
Incontinence/moisture – urine, faeces and sweat can cause skin damage, so it is essential to keep your skin clean and dry. You should ensure you follow these principles:
- go to the toilet often
- if you require a continence product a nurse will assess you to find the correct product for your needs
- wash your skin with non-perfumed soap, preferably pH balanced, pat skin dry. You may require a barrier product to protect your skin.
- avoid oil-based creams such as Sudocrem, Metanium or Conotrane if you wear continence products, as they can affect absorbency of the product
You can help to prevent avoidable pressure ulcers by following the above guidance.
A series of local factsheets have been produced by NHS Western Isles to help support people with pressure ulcers. This includes titles such as ‘How to look after your leg ulcer', ‘How to look after your wound' and ‘Preventing pressure areas', all available via: www.wihb.scot.nhs.uk/our-services/nurse-led-services/tissue-viability-nurse-service/
If you have any pressure concerns, please make an appointment with your GP or visit www.nhsinform.scot for further information.
Everyone is responsible for preventing pressure areas. Together we can do it!
- NEXT PAGE: Sitemap
- LAST REVIEWED ON: November 16, 2020