Heading 2
Before your appointment, you may be asked to:
- have blood tests to check your HbA1c (average glucose over 2-3 months), and sometimes bloods to check kidney function, cholesterol and thyroid
- have blood pressure, height and weight checked, and urine check surgery (if arranged before hand)
- bring your continuous glucose monitor (CGM) reader and/or blood glucose diary
- bring a list of your medications.
During your diabetes review:
- The Practice Nurse or DSN will review your HbA1c result. A target HbA1c may be discussed at clinic. Discussion of glucose readings, time in range and any recent hyperglycaemia (high glucose) or hypoglycaemia (low glucose) episodes. Medication or insulin may be adjusted if necessary.
- A review of any other blood tests including thyroid function, kidney function, urine microalbuminuria (Urine Albumin to Creatinine Ratio – ACR).
- A review of your blood pressure, as high blood pressure increases the risk of heart and kidney problems, a target blood pressure may be set.
- Discussion regarding your wellbeing. Including weight, diet, physical activity, alcohol, smoking and emotional wellbeing. You can raise any concerns about managing diabetes.
- A foot check examination. This is to check circulation, nerve sensation, skin conditions and ulcers to reduce risk of serious foot complications.
- Check you are up-to- date with your eye screening (Diabetic Retinal Screening).
What is diabetic retinopathy?
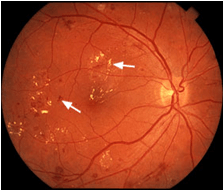
Picture of Diabetic Retinopathy
Diabetic Retinopathy is a condition that occurs when diabetes affects the small blood vessels in the retina, which is at the back of the eye. The blood vessels in the retina can leak or become blocked.
This condition may cause blindness or serious damage to your eyesight. In its early stages there are no symptoms so you may not realise that you have diabetic retinopathy.
Why should I be screened?
If you have diabetes then screening is important because your eyes are at risk of damage from diabetic retinopathy. Screening is a key part of your diabetes care and can reduce that risk by detecting the condition early before you notice any changes to your sight.
Untreated diabetic retinopathy is the most common cause of sight loss in people of working age. When the condition is caught early, treatment is effective at reducing or preventing damage to your sight.
Useful after-care eye drop guidance has been produced aimed at those who receive eye drops (Tropicamide 1%) during
their Diabetic Eye Screening appointment. Click here to view.
Further information
For further information, to request an appointment or support to attend, please contact the Diabetes Centre by telephoning 01851 708327 or 01851 708331.
You can also find further information on the NHS Inform website.
Please be aware that if you have any problems or concerns related to your feet health, you can access the NHS Western Isles Podiatry Department website for further information and advice or on how to contact them. Visit: www.wihb.scot.nhs.uk/our-services-podiatry
Holiday Foot Care
Going on holiday can cause foot problems, so follow these simple precautions to ensure a trouble-free time.
The Journey
Long journeys on trains, buses and planes can make your feet swell. Walk up and down the aisle every half hour – the exercise will help keep the swelling down. Make sure your shoes don't become too tight.
Footwear
If you normally wear hospital supplied shoes, wear them on holiday too. Remember that changing over to ordinary shoes could cause an ulcer – and ruin your holiday.
Avoid walking barefoot. On the beach, and in the sea, wear plastic sandals.
Sunburn
Avoid sunburn to your feet and legs. Use a sun screen with a high protection factor – or keep covered.
Foot Care
If your skin gets very dry in the hot weather, you may need to apply more moisturising cream than usual. Pay special attention to your heels – dry skin here cracks easily.
First Aid
Take small sterile dressings, antiseptic and adhesive tape on holiday. Clean any small blisters, cuts or grazes thoroughly then apply a sterile dressing.
Foot Check
Examine your feet daily for sores, swelling and colour changes. If any of these problems develop, then visit the local state registered podiatrist or doctor.
Remember: delays in seeking treatment may make foot problems worse. Seek early treatment for all holiday foot problems.
Foot Screening for People with Diabetes
Diabetes can have an effect on the blood and nerve supply, which can lead to complications in the leg and foot. This can slow down the healing process in the body and reduce the sensation to pain, temperature and pressure. Not everyone will develop these problems, but ALL people with diabetes should follow the same rules of foot care to prevent problems developing.
Maintaining good blood sugar and weight control is very important, as is avoiding smoking.
Your Annual Foot Check
As part of your ongoing diabetes care you will receive a formal check of your feet at least once a year. This includes checking the pulses and feeling in your feet. This will be undertaken by whoever is providing your diabetes care and may be a doctor, nurse or podiatrist. This will allow them to calculate your risk of developing a foot ulcer in the future which could be low, medium or high. You can ask your GP, nurse or podiatrist to tell you what your risk score is and they will provide you with a leaflet specially written for that risk category.
Inspect Your Feet Daily
- Look especially in between your toes and around your heels.
- If you cannot bend over, ask a friend or relative to help, or put a mirror on the ground.
- Be aware of any blisters, breaks in the skin, pain or any signs of infection such as swelling, heat or redness.
Tell your Diabetes team or Podiatrist about any changes in your feet.
Free leaflets are available to view/download from Diabetes UK. Click here to view.
- NEXT PAGE: Diabetes Department - What to do if…
- LAST REVIEWED ON: March 3, 2026